Leave message
Can’t find what you’re looking for?
Fill out this form to inquire about our custom protein services!
Inquire about our Custom Services >>
































 Limited Edition Golden Llama is here! Check out how you can get one.
Limited Edition Golden Llama is here! Check out how you can get one.  Limited Edition Golden Llama is here! Check out how you can get one.
Limited Edition Golden Llama is here! Check out how you can get one.
 Offering SPR-BLI Services - Proteins provided for free!
Offering SPR-BLI Services - Proteins provided for free!  Get your ComboX free sample to test now!
Get your ComboX free sample to test now!
 Time Limited Offer: Welcome Gift for New Customers !
Time Limited Offer: Welcome Gift for New Customers !  Shipping Price Reduction for EU Regions
Shipping Price Reduction for EU Regions
> Insights > Unleashing Full Potential of iPSC Derived Allogeneic Cell Therapies Induced pluripotent stem cells (iPSCs) has catalyzed a paradigm shift in cellular immunotherapy. Through reprogramming of somatic cells into a pluripotent state, iPSCs provide a renewable source for deriving diverse cell lineages, including T cell, natural killer (NK) cells, and macrophage. This capability holds profound implications for the advancement of allogeneic “off-the-shelf” cell therapies derived from healthy donor resources circumventing constraints associated with autologous patient-derived products.
Conventional autologous chimeric antigen receptor (CAR) T cell therapies have revolutionized immunotherapy but have countered challenges such as limited patient starting material, suboptimal T cell fitness, and a complex, costly manufacturing process. iPSC technology offers an alternative avenue to overcome these bottlenecks by enabling the derivation of therapeutic T cells from healthy donor sources. The process involves somatic cell reprogramming followed by directed differentiation toward hematopoietic progenitor cells (HPCs). These HPCs are then cultured under specific conditions, including the exposure to Notch ligands like DLL4, and cytokines cocktails (IL-2, IL-7, IL15 and others) to mimic the thymic environment essential for T cell maturation. Once differentiated, the iPSC-derived T cells can undergo CAR engineering to redirect specificity against tumor-associated antigens (TAAs).
Beyond manufacturing advantages, allogeneic iPSC-derived CAR-T products have several therapeutic benefits over autologous counterparts. Master iPSC banks enable consistent, scalable production under Good Manufacturing Practice (GMP) conditions. The healthy donor origin may produce superior cellular fitness, persistence, and anti-tumor potency compared to patient T cells. Moreover, multi-antigen CAR targeting enhances tumor epitope coverage, while genomic removal of endogenous T cell receptors (TCRs) and human leukocyte antigen (HLA) molecules mitigates graft-versus-host disease (GvHD) risk.
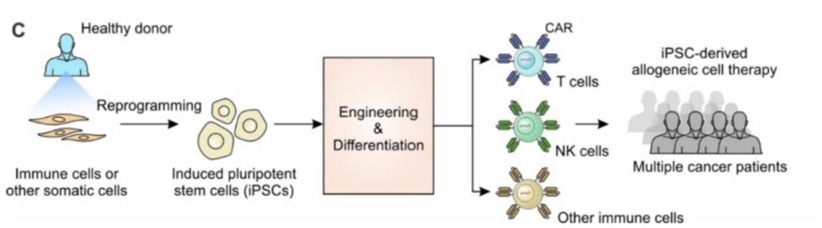
Figure 2. Schemic illustration of 2D and 3D protocol for iPSC differentiation to NK cells
iPSC-derived NK cell therapy presents another promising therapeutic avenue, leveraging the innate ability of the NK cells and the unlimited expansion potential of iPSCs. Unlike autologous CAR-T, iPSC-NK cells originate from healthy donors and can be consistently manufactured through directed differentiation toward the lymphoid lineage. Mimicking in vivo NK cell development, the differentiation of iPSCs into NK cells typically involves cytokines and growth factors that mirror natural NK cell development. Recent advancements have led to feeder-free differentiation protocols, simplifying the process, and improving scalability. These methods entail stepwise exposure to growth factors such as BMP4, VEGF, SCF, Flt3-L, IL-3, IL-7, and IL15, along with stromal support, guiding iPSCs through stages of HPCs to functional cytotoxic CD56+CD3- NK cells. These allogeneic NK cells possess direct cell-mediated tumor cytotoxicity, antibody-dependent cell-mediated cytotoxicity (ADCC) and can be engineered with CARs for HLA-independent tumor targeting. Notably, the NK cell lineage offers a favorable safety profile relative to T cells, with reduced propensity for cytokine release syndrome (CRS), neurotoxicity, and GvHD.
The future of allogeneic NK cell therapy looks promising, with ongoing research focused on enhancing efficacy, safety, and applicability in hematological and solid tumor indications. Efforts aim to improve homing, persistence, and tumor infiltration of iPSC-derived NK cells, as well as to minimize rejection risk in allogeneic settings. The development of CAR-NK cells, combining CAR technology with the innate cytotoxicity of NK cells, represents a significant advancement of next generation immunotherapy. Overall, engineered NK cells could offer a safer and potentially more effective alternative to CAR-T cell therapy, especially for immunosuppressive solid tumors.
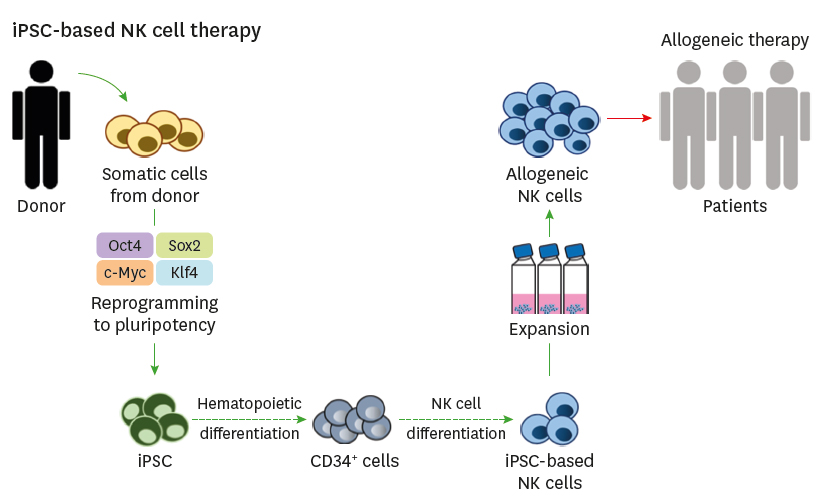
Figure 2. iPSC-derived NK cell therapy schematic diagram. Immune Netw. (Shin) 2020;20(2):e14.
Building upon the success of T and NK cell engineering platforms, iPSCs offer the potential to generate a novel class of cellular immunotherapies—CAR-macrophages (CAR-Ms). CAR-M therapies harness the inherent abilities of macrophages, which are versatile innate immune cells capable of phagocytosis, tissue remodeling, and exerting anti-inflammatory effects. These engineered macrophages can be redirected to target and eliminate cancer cells, presenting a promising new platform for treating a variety of malignancies, including hematological and solid tumors.
Through directed differentiation along the myeloid lineage, renewable iPSC can generate mature CD14+CD16+ macrophages by culturing HPCs with growth factors including GM-CSF, M-CSF, IL-3, and IL-4. These phagocytic macrophages can then genetic modification to express CARs, redirecting their cytotoxic, antigen-presenting, and immunomodulatory functions toward defined TAAs.
However, the field of CAR-M therapy is still in its nascent stages, and several challenges and limitations need to be addressed. One of the primary concerns is the potential for the immunosuppressive tumor microenvironment (TME) to subvert the anti-tumor functions of CAR-Ms, although preclinical models suggest that CAR-Ms may possess the ability to reprogram the TME. The efficacy of CAR-Ms as a monotherapy is still uncertain, and combination therapies with other forms of cancer immunotherapy, such as checkpoint inhibitors or CAR-T, may be necessary to overcome the complexities of the TME and achieve better therapeutic outcomes. Additionally, the manufacturing processes, cryopreservation techniques, and repeated dosing regimens for CAR-Ms require optimization to maintain robust and persistent anti-tumor surveillance.
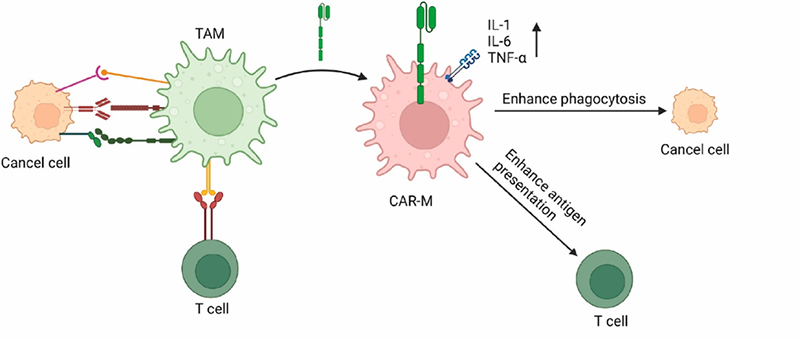
Figure 3. CAR-M enhances the anti-tumor cells by increasing expression of inflammatory factors, phagocytosis and antigen presentation ability to T cells. Differentiation (Hang). 2023; 130:51-57
The development of iPSC technology has revolutionized cellular immunotherapy by providing a sustainable source for deriving various immune effector cells from healthy donor sources. As these versatile allogeneic cell therapy platforms progress through clinical testing, they hold immense promise for transforming the treatment landscape for both hematological and solid cancers, potentially offering effective and better-tolerated immunotherapies for a wide range of indications.
We are committed to the development of high-quality cell culture reagents crucial for development of clinical stage of immune cell therapy. Employing a stringent GMP-grade quality management system, we have successfully developed an array of high-quality GMP grade growth factors, including DLL4, VEGF, Flt-3L, SCF, IL-2, IL-7, IL15 and more, specifically designed to support iPSC-derived cell therapy development and large-scale clinical manufacturing.
1. Zhou Y, Li M, Zhou K, Brown J, Tsao T, Cen X, Husman T, Bajpai A, Dunn ZS, Yang L. Engineering Induced Pluripotent Stem Cells for Cancer Immunotherapy. Cancers (Basel). 2022 May 1;14(9):2266. doi: 10.3390/cancers14092266. PMID: 35565395; PMCID: PMC9100203.
2. Goldenson BH, Hor P, Kaufman DS. iPSC-Derived Natural Killer Cell Therapies - Expansion and Targeting. Front Immunol. 2022 Feb 3;13:841107. doi: 10.3389/fimmu.2022.841107. PMID: 35185932; PMCID: PMC8851389.
3. Sloas C, Gill S, Klichinsky M. Engineered CAR-Macrophages as Adoptive Immunotherapies for Solid Tumors. Front Immunol. 2021 Nov 24;12:783305. doi: 10.3389/fimmu.2021.783305. PMID: 34899748; PMCID: PMC8652144.
4. Wang C, Liu J, Li W. 'Off the shelf' immunotherapies: Generation and application of pluripotent stem cell-derived immune cells. Cell Prolif. 2023 Apr;56(4):e13425. doi: 10.1111/cpr.13425. Epub 2023 Mar 1. PMID: 36855955; PMCID: PMC10068955.
5. Kao C-Y, Mills JA, Burke CJ, Morse B, Marques BF. Role of Cytokines and Growth Factors in the Manufacturing of iPSC-Derived Allogeneic Cell Therapy Products. Biology. 2023; 12(5):677. https://doi.org/10.3390/biology12050677
6. Hang S, Wang N, Sugimura R. T, NK, then macrophages: Recent advances and challenges in adaptive immunotherapy from human pluripotent stem cells. Differentiation. 2023 Mar-Apr;130:51-57. doi: 10.1016/j.diff.2023.01.001. Epub 2023 Jan 18. PMID: 36682340.
7. Shin MH, Kim J, Lim SA, Kim J, Kim SJ, Lee KM. NK Cell-Based Immunotherapies in Cancer. Immune Netw. 2020 Mar 9;20(2):e14. doi: 10.4110/in.2020.20.e14. PMID: 32395366; PMCID: PMC7192832.
This web search service is supported by Google Inc.