Leave message
Can’t find what you’re looking for?
Fill out this form to inquire about our custom protein services!
Inquire about our Custom Services >>

































 Limited Edition Golden Llama is here! Check out how you can get one.
Limited Edition Golden Llama is here! Check out how you can get one.  Limited Edition Golden Llama is here! Check out how you can get one.
Limited Edition Golden Llama is here! Check out how you can get one.
 Offering SPR-BLI Services - Proteins provided for free!
Offering SPR-BLI Services - Proteins provided for free!  Get your ComboX free sample to test now!
Get your ComboX free sample to test now!
 Time Limited Offer: Welcome Gift for New Customers !
Time Limited Offer: Welcome Gift for New Customers !  Shipping Price Reduction for EU Regions
Shipping Price Reduction for EU Regions
> Insights > Interpreting the Association Between Cytokines and Autoimmune Diseases--Topic 3 Cytokines are important protein mediators of immunity, inflammation, cell behavior. Given that these are the main biological processes involved in autoimmunity, there is evidence that cytokines play an important role in the pathogenesis of autoimmune diseases.
In Topic 1 and Topic 2, we have examined the connection between cytokines and 6 major autoimmune diseases. These diseases are closely linked to cytokine imbalance. However, with over 100 refractory AIDs discovered, overcoming them remains difficult. This issue, we will explore the connections between cytokines and three other autoimmune diseases.
Ankylosing Spondylitis
Psoriatic arthritis
Systemic Sclerosis
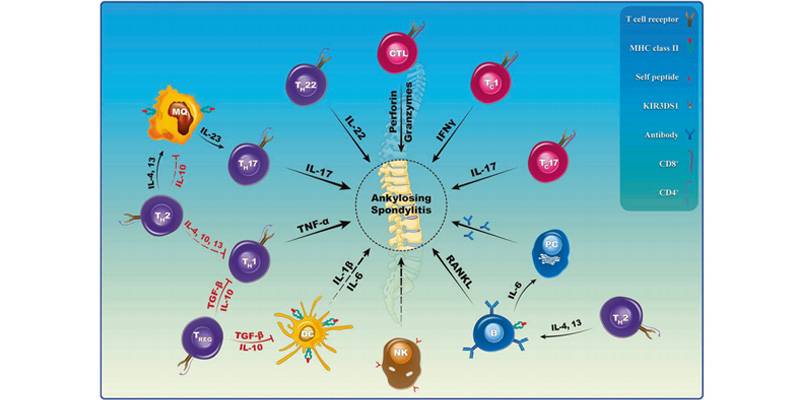
The pathogenesis of ankylosing spondylitis (AS) is closely related to dysregulation of immune function, where the abnormal release of inflammatory factors and imbalance of immune cells play crucial roles in the disease process.
Excessive levels of cytokines such as TNF-α, IL-17, and IL-23 can promote inflammatory responses and accelerate joint damage. Monoclonal antibody drugs targeting these key cytokines, such as adalimumab, etanercept, secukinumab, and guselkumab, have become important cytokine-targeted therapies for the treatment of AS. Furthermore, IL-6 inhibitors have also demonstrated promising clinical efficacy in recent years, offering the potential to fundamentally curb disease progression.
In summary, precisely modulating key inflammatory factors may provide an effective means to control the development of AS and improve patient prognosis.
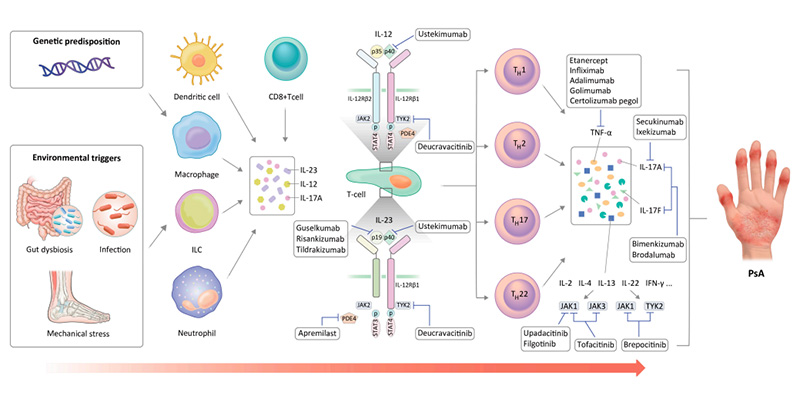
Psoriatic arthritis (PsA) is a chronic inflammatory disease that can lead to joint destruction and deformities, significantly impacting the patient's quality of life. With a deeper understanding of the pathological mechanisms of PsA, new treatment options have emerged, which have opened up new directions for the management of PsA.
• TNF-α Inhibitors
TNF-α is the most potent proinflammatory cytokine known to date and plays a critical role in PsA. TNF-α inhibitors can significantly alleviate symptoms in patients. Currently, there are five TNF-α inhibitors approved by the FDA for the treatment of PsA: infliximab, etanercept, adalimumab, golimumab and golimumab.
These TNF-α inhibitors have demonstrated efficacy in managing the symptoms and progression of PsA.
• IL-17 Inhibitors
IL-17A is a member of the IL-17 cytokine family and plays a critical role in the skin lesions, arthritis, and enthesitis associated with PsA. Several IL-17 inhibitors are currently in development, and two have been approved by the FDA for the treatment of PsA: secukinumab and ixekizumab.
These IL-17 inhibitors have demonstrated efficacy in managing the various manifestations of PsA by targeting this key inflammatory cytokine.
• IL-12/IL-23 Inhibitors
The IL-12/IL-23 axis is an important pathological pathway in the development of psoriatic arthritis (PsA). Targeting the IL-23p19 subunit, the related inhibitor tildrakizumab is currently in phase III clinical trials. The IL-12/IL-23 inhibitors that have been approved by the FDA for the treatment of PsA include: ustekinumab, guselkumab and risankizumab.
These therapies that block the IL-12/IL-23 signaling have shown efficacy in managing the diverse manifestations of PsA by intervening in this key inflammatory pathway.
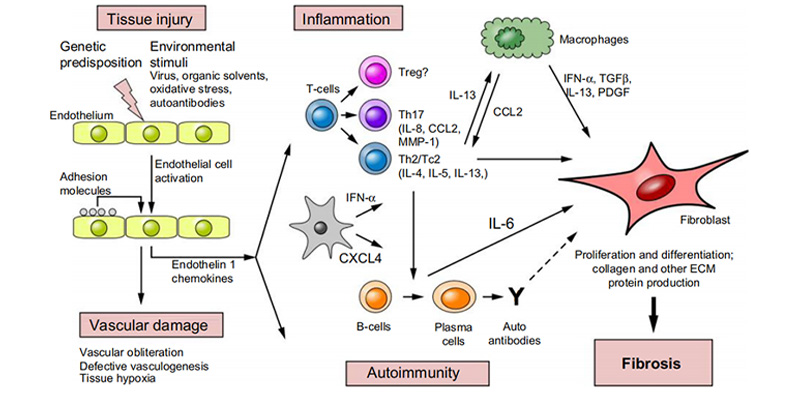
Systemic Sclerosis (SSc) is a rare systemic autoimmune disease characterized by a high degree of clinical heterogeneity. Immune cells release a variety of cytokines and growth factors, which are believed to play key roles in the inflammatory and fibrotic processes of SSc.
Cytokines such as IL-1, IL-4, IL-13, IL-17, IL-23, and IL-31 are involved in regulating the inflammatory, vascular, and fibrotic processes in SSc, making them potential therapeutic targets. Elevated IL-6 levels are closely associated with poor prognosis, also making it a potential target for SSc treatment.
Therapies targeting the TGF-β pathway, such as fresolimumab, have entered phase I clinical trials, brodalumab, an IL-17 inhibitor that can induce vascular disease, inflammation, and fibrosis, has also entered phase III clinical trials.
Additionally, inhibiting IL-1, IL-31, and interferon signaling pathways have shown promising prospects for the treatment of SSc.
ACROBiosystems is providing you with a series of recombinant cytokines and their receptors, including Interleukins, Growth Factors, TNFs, Chemokines, CSFs, IFNs, and Complement Components with high purity, high bioactivity, and high batch-to-batch consistency to accelerate your autoimmune diseases drug development programs.
We have launched ClinMax™ ready-to-use ELISA kits with rigorously quality control, ensuring the precision, stability, and consistency of the analysis results, to better meet your experimental needs.
This web search service is supported by Google Inc.